A 45 year old female , an agricultural labour by occupation came to the casualty with the chief complaints of-
HOPI–
The patient was apparently asymptomatic one month back and then developed fever,Which was high-grade, associated with chills, and was taken to a local hospital and got treated. Along with fever, she had loss of appetite and loss of taste. Fever subsided for one day and then she developed it again.
She visited the hospital after 15 days, Where they advised her to consult a gynaecologist as she had her last LMP2 years back
She never had any complaints of pain abdomen
Then, she consulted a gynaecologist, and the doctor advised her USG for the localisation of infection. The USG revealed a right ovarian cyst. Along with USG ,haemogram, RFT, LFT were done. RFT showed all the values Within the normal range with creatinine being around 0.9-1 ,Haemoglobin was normal. Apart from having right ovarian cyst, she has no other findings. So, the patient was referred to a general surgeon. The size of the variant cyst was about 8 cm and the doctors thought to operate it. They scheduled the surgery on 11/7/21 and patient had been to the hospital on 9/7/21 For pre-anaesthetic checkup. So, on that day her HB was 10, and then she underwent two units of PRBC transfusion. The patient was scheduled to get operated on 11/7/21 at 3:00 pm. When the patient was in the OT and put on foley’s And all the anaesthetic medications were given but on opening the abdomen, she had subcutaneous edema and And the fluid Was gushing out of it. The doctors were not sure where the fluid was coming from, whether it’s from the right ovarian cyst or peritoneum.
Assuming it to be the peritoneal fluid, it was thought to be ascites,And ascitic fluid analysis was sent
Patient had TB 15 years back, assuming it to be abdominal TB, samples were sent for AFB and gram stain
Then, she came to the casualty of Kims on 15/7/21 at 9 PM saying that she needs to undergo dialysis and the patient was referred to this hospital in view of further haemodialysis to be done.
When she presented to the casualty, she did not have any pedal edema or SOB
PAST HISTORY-
Not a known case of diabetes mellitus and hypertension
Known case of pulmonary Koch’s disease 15 years back and used antitubercular drugs for one year
PERSONAL HISTORY-
Diet – mixed
Sleep – adequate
Appetite – lost
Bowel and bladder – decreased urine output
No addictions
FAMILY HISTORY-
No relevant family history
GENERAL EXAMINATION-
Patient is conscious, coherent, cooperative
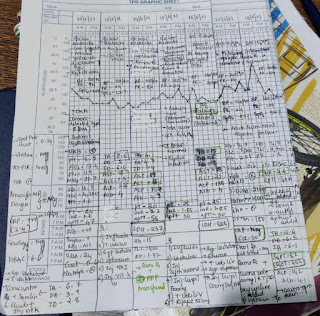
VITALS-
TEMP-afebrile
BP-110/70 mmhg
RR-22 cpm
PR-82bpm
Pallor- Present
No icterus, cyanosis,clubbing,lymphadenopathy,edema of feet
SYSTEMIC EXAMINATION-
PER ABDOMEN-
INSPECTION-
Abdomen is distended with transverse umbilicus
No engorged veins are seen
PALPATION-
There is no organomegaly
PERCUSSION-
Shifting dullness is present
Ascitic fluid analysis was done
The SAAG is 0.98
CVS-
S1,S2 heard
No thrills and murmurs
RESPIRATORY-
BAE +
NVBS heard
Trachea is central in position
CNS-
No focal neurological deficit
Gynaecology referral was done
Recent gynaecology referral-
They advised to talk to oncosurgeon, who advised CECT for her to look for any cervical lymphadenopathy but it turned out to be clueless
CAUSE OF AKI?
Perioperative AKI does not arise from a single insult, but instead develops as a result of several, with hypoperfusion and inflammation thought to be the main drivers.[1] Perioperative AKI is due to inflammation caused by hemodynamic instabilities, nephrotoxicity, damage-associated molecular pattern (DAMP), and obstruction.[3] Decrease in mean arterial pressure (MAP) due to hypovolemia or systemic effects of anesthetics contribute to renal hypoperfusion. Once the intrinsic compensatory mechanisms of the kidneys, mediated through sympathetic nervous system activation leading to the production of antidiuretic hormone and angiotensin-II, are surpassed, the kidneys are unable to maintain an adequate glomerular filtration rate (GFR) and renal function is reduced. In patients with underlying chronic renal disease, autoregulation is impaired, exacerbating the effects of hypoperfusion. Additionally, surgical stimulation induces systemic inflammation leading to microcirculatory effects, endothelial dysfunction, and increased leukocyte migration. The net result of these inflammatory changes is damage to the renal tubules and AKI.[1]
https://www.ncbi.nlm.nih.gov/books/NBK557677/
CAUSE OF ASCITES?
FURTHER PLAN
INVESTIGATIONS-
CT REPORT-
ULTRASOUND REPORT-
Perioperative AKI(Pre-Renal/Renal)
Ascitis secondary to ?abdominal kochs
Right ovarian cyst (?Benign)
K/c/o pulmonary koch’s 15 years back