18 year old male patient elog
A 18 year old male,from miryalaguda,who is a student, came to the hospital with chief complaints of low backache 1 week ago,fever since 5 days ,yellowish discolouration of eyes since 3 days ,vomitings (2 episodes) and loose stools(3 episodes)and blood tinged urine yesterday morning
HISTORY OF PRESENT ILLNESS-
Patient was apparently asymptomatic 6 months ago,then he noticed gradual loss of weight since 6months,patient had history of polyuria,nocturia,polydypsia since 2 months
10 days ago, patient attended a function outside and after 2 days he developed low backache and 2 episodes of vomitings and 3 episodes of loose stools for one day which subsided on its own.
Next day,patient developed fever,intermittent,high grade,subsided with medication. Patient went to RMP and got treated for fever.patient noticed yellowish discolouration of eyes and urine 3 days ago.Nausea and loss of appetite +
Burning micturition is present
PAST HISTORY-
No history of diabetes,asthma,TB ,epilepsy
PERSONAL HISTORY-
Diet-mixed
Appetite-lost
Bowel and bladder-regular
Sleep-adequate
FAMILY HISTORY-
No relevant family history
GENERAL EXAMINATION-
Patient is conscious,coherent and cooperative
VITALS-
Temp-
BP-110/70 mm Hg
PR-94
RR-24
Pallor- absent
Icterus-present
Cyanosis-absent
Lymphadenopathy-absent
Clubbing-absent
Oedema-absent
SYSTEMIC EXAMINATION
CVS-
S1,S2 heard
No murmurs
No thrills
RESPIRATORY-
Bilateral air entry with normal vesicular breath sounds,no wheeze,no dyspnea ,position of trachea is central
ABDOMEN-
Shape-scaphoid
Tenderness in right hypochondrium,epigastrium
No palpable mass, free fluid,no bruit
Liver and spleen- not palpable
Bowel sounds-present
PROVISIONAL DIAGNOSIS-
acute viral hepatitis
Denovo DM type 1
DKA
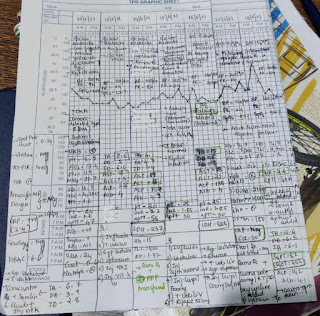
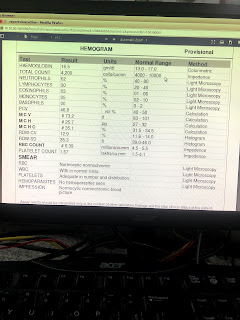
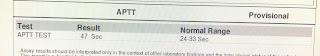
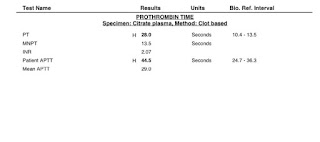
INVESTIGATIONS-
Update on day 5-
Subjectively-c/o lethargy from today afternoon. Did not pass urine the entire day.
Objectively- pt is drowsy not responding to verbal commands, responding to painful stimulus , giving bizarre starey looks occasionally.
BP-110/70
PR-70bpm regular normal volume
Abdomen- Palpable bladder
Assessment- ? Absence seizure / ? Intra parenchymal bleed
Plan-sr electrolytes sent
CT brain planned now
Update on day 6-
Acute liver failure with ?acute pancreatic failure
?Hepatic encephalopathy
Indirect hyperbilirubinemia-? Criggler najjar syndrome
?hepatic coagulopathy
?porphyria
Diabetic ketoacidosis (resolved)
?denovo diabetes type 1
Patient became drowsy and not responding to verbal communication since yesterday evening with acute retention of urine,bizarre starey looks, responding to painful stimuli
?absence seizure
Inj. Loraz 2cc given yesterday night
CT brain done- normal
O/E-
GCS-E2 V2 M3
Pupils-B/L RL dilated
BP -130/80 mmHg
PR-70 bpm
Temp- 100F
CVS- S1,S2 heard
RS- BAE
UPDATE ON DAY 10-
His repeat LFT
TB 14.3
Indirect bilirubin 4.6
DB 9.6
SGOT 190
SGPT 750
ALP 113
TP 6.2
*Alb 2.5*
Glb 3.7
A/G 0.6
Serum ammonia :108 (Normal range)
Urine for porphobilinogen negative
Yesterday night he had one more episode of ?absence seizure where he had loss of awareness of surroundings with staring look and repeating a single word for about 15mins
**covid antibodies positive
Update on day 13-
discharge summary-
Date:29/6/21
Ward:GENERAL MEDICINE
Unit:5
NAME OF THE TREATING FACULTY-
DR.E.SAI NIKITHA (INTERN)
DR.SRAVANI(INTERN)
DR.KRUPALATHA(INTERN)
DR.TEJASWINI(INTERN)
DR.RAMYA(INTERN)
DR.VAISHNAVI(PGY2)
DR. CHANDANA (PGY1)
DR. ARJUN(AP)
DR.HAREEN(SR)
DR. RAKESH BISWAS(HOD)
DIAGNOSIS-
ACUTE FULMINANT HEPATIC FAILURE SECONDARY TO ?POST INFECTIOUS(VIRAL/ BACTERIAL) ? TOXIN MEDIATED ? MISC
WITH HEPATIC ENCEPHALOPATHY
COAGULOPATHY
METABOLIC SEIZURES (? ABSENCE SEIZURES)
DKA RESOLVED
? DENOVO TYPE 1 DM
WITH THROMBOCYTOPENIA
CASE HISTORY AND CLINICAL FINDINGS-
Patient was apparently asymptomatic 6 months ago,then he noticed gradual loss of weight since 6months,patient had history of polyuria,nocturia,polydypsia since 2 months
10 days ago, patient attended a function outside and after 2 days he developed low backache and 2 episodes of vomitings and 3 episodes of loose stools for one day which subsided on its own.
Next day,patient developed fever,intermittent,high grade,subsided with medication. Patient went to RMP and got treated for fever.patient noticed yellowish discolouration of eyes and urine 3 days ago.Nausea and loss of appetite +
Burning micturition is present
no h/o pain abdomen
blood tinged urine since 1 day
no h/o previous similar complaints
pt. got investigated outside (8/6/21)-
RBS-360MG/DL
(11/6/21)-TB-6.7
DB-3.9
ID-2.8MG/DL
pt. is using tab. glimy M1 since 3 days
VITALS-
TEMP-100.5F
PR-94/BPM
BP-110/70 MMHG
SPO2-100%
GRBS-211 MG%
CVS-
S1,S2 HEARD
RS-
BAE+
P/A-
TENDERNESS PRESENT IN RIGHT HYPOCHONDRIUM AND EPIGASTRIUM
INVESTIGATIONS-
CECT ABDOMEN -FATTY LIVER , NORMAL CBD ,NO IHBRD ,MILD ASCITIS ,INCIDENTALLY DETECTED SMALL BOWEL INTUSUSSCEPTION
CT BRAIN NORMAL
TREATMENT GIVEN-
COURSE IN THE HOSPITAL-
18 YEAR OLD MALE CAME WITH C/O LBA ,YELLOWISH DISCOLORATION OF EYES,FEVER SINCE 4-5 DAYS PT. WAS ADMITTED AND NECESSARY INVESTIGATIONS WERE SENT. PT WAS FOUND TO HAVE ISOLATED HYPERBILIRUBINEMIA(6.7TB )PREDOMINANTLY INDIRECT AND ENZYMES WERE NORMAL .HIS URINE FOR KETONES WERE POSITIVE WITH RBS 280 AND MILD ACIDOSIS .SO TH PT WAS DIAGNOSED AND TREATED AS DKA (DENOVO DETECTED TYPE 1DM),INDIRECT HYPERBILIRUBINEMIA UNDER EVALUATION,WITH COAGULOPATHY.USG ABDOMEN -LIVER NORMAL ECHOTEXTURE,CBD NORMAL ,NO EVIDENCE OF IHBRD
DAY1-
PT WAS TREATED WITH INSULIN AND IV FLUIDS,VIT K
DAY2-
HIS SUGARS CAME INTO CONTROL ON DAY2 OF ADMISSION .HIS INSULIN REQUIREMENT WAS AROUND 12 UNITS ACTRAPID PER DAY .PT CONTINUED TO HAVE LBA
XRAY LS SPINE WAS DONE WHICH WAS NORMAL
DAY3-
PT COMPLAINS OF LBA AND LOSS OF APPETITE AND DID NOT PASS STOOLS SINCE 1 DAY
SUPPORTIVE MANAGEMENT WAS GIVEN ,SYP LACTULOSE WAS GIVEN
DAY4-
PT COMPLAINED OF SEVERE GENERALISED WEAKNESS
BY AROUND EVNG 6 PM , PT BECAME DROWSY NOT RESPONDING TO VERBAL COMMANDS(?HEPATIC ENCEPHALOPATHY) WITH ACUTE RETENTION OF URINE AND BIZARRE STAREY LOOKS ,RESPONDING TO PAINFUL STIMULI ?ABSENCE SEIZURES ,INJ. LORAZ 2CC GIVEN
IN VIEW OF COAGULOPATHY CT BRAIN WAS DONE TO RULE OUT IC BLEED
CT BRAIN NORMAL
PT DID NOT PASS STOOLS SINCE 2 DAYS ,ENEMA WAS GIVEN
PT PASSED STOOLS AFTER ENEMA
FOLEYS CATHETERISATION WAS DONE ,COLA COLORED URINE OF ABOUT 1000 ML WAS COLLECTED IN UROBAG
URINE WAS SENT FOR ANALYSIS ,URINE FOR PORPHOBILINOGEN NEGATIVE ,NO RBCs IN URINE
UROLOGY REFERRAL WAS TAKEN IN VIEW OF 5MM RIGHT RENAL CALCULUS ,ADVISED FOR XRAY KUB AFTER STABILISATION
DENGUE SEROLOGY NEGATIVE,SMEAR FOR MP NEGATIVE
DAY5-
GCS- E2V2M3
PT COMATOSED WITH B/L REACTING PUPILS ,DILATED
VITALS STABLE ,DEEP TENDON REFLEXES NORMAL WITH B/L EXTENSOR PLANTAR
WITH SUSPICION OF CEREBRAL MALARIA ,INJ.FALCIGO 120 MG STAT. GIVEN(0----12---24--48 HRS), 4 DOSES GIVEN,INJ. LEVIPIL 500 MG BD WAS STARTED ,INJ. DOXYCYCLINE 100 MG BD WAS STARTED
OTHER SUPPORTIVE MEASURES WERE GIVEN SUCH AS IV FLUIDS ,SYP.LACTULOSE,ENEMA WERE GIVEN
HIS TB SHOOT UP TO 15 ,DB 6,IB 9,AST 18,ALT 22 ,ALP 138,TP 7.6,ALB 4,HB 13,(IT WAS 16 GM AT THE TIME OF ADMISSION )
DIFFERENTIAL DIAGNOSIS-
?CEREBRAL MALARIA
?ACUTE HEMOLYSIS(INTRAVASCULAR)
? ACUTE LIVER FAILURE (TOXIN MEDIATED)
? ACUTE INTERMITTENT PORPJHYRIA
HEPATIC ENCEPHALOPATHY WITH METABOLIC SEIZURES AND COAGULOPATHY
DKA (RESOLVED),DENOVO DETECTED ?TYPE 1 DM
DAY 6-
GCS-E2V1M3 WITH B/L REACTIVE PUPILS AND VITALS STABLE
SERUM LDH-237
SERUM IRON 150 ,SERUM FERRITIN> 1500,HBA1C 6.6,TSH 1
TRIPLE PHASE CT ABDOMEN WAS DONE TO RULE OBSTRUCTIVE PATHOLOGY WHICH SHOWED FATTY LIVER NO IHBRD ,NORMAL CBD ,NORMAL HEPATIC VEINS IVC,INCIDENTALLY DETECTED SMALL BOWEL INTUSUSSCEPTION
PERIPHERAL SMEAR -NORMOCYTIC,NORMOCHROMIC
SICKLING TEST NEGATIVE
FREE T3 3.86,FREE T4-1.41
D DIMER 2160
DAY 7-
GCS-E2V2M3
SUSPICION OF FUNGAL HEPATITIS ,INJ. FLUCONAZOLE 200 MG IV OD WAS STARTED ,INJ. CEFTRAIXONE 1 GM IV BD STARTED
IN VIEW OF UNEXPLAINED LIVER FAILURE N ACETYL CYSTEINE ,IV INFUSION WAS STARTED (600 MG)
WITH SUSPICION OF ANY CEREBRAL EDEMA ,3% NACL INFUSION WAS GIVEN FOR 1 DAY
GASTROENTEROLOGY REFERRAL WAS TAKEN : ACUTE FULMINANT HEPATIC FAILURE ,ADVISED FOR LIVER TRANSPLANTATION BUT PT ATTENDERS WERE NOT AFFORDABLE
DAY 8-
GCS-E1V1M3,VITALS STABLE
IN VIEW OF ACUTE FULMINANT LIVER FAILURE, HEPATIC ENCEPHALOPATHY PROBABILITY OF MULTISYSTEM INFLAMMATORY SYNDROME (POST COVID) WAS CONSIDERED .COVID ANTIBODIES WERE SENT WHICH SHOWED COVID ANTIBODY IGG >150(NORMAL IS <1),COVID ANTIBODY TOTAL VIA ELISA 5.85(NORMAL IS <0.8)
TB-12.6,DB-6.5,IB-6.1,AST 402,ALT 82 ,TP 6.8,ALB 4.1,HB 12.6,TLC5300,PLT 1.31
BY EVNG 7 PM PT SENSORIUM IMPROVED DRASTICALLY, PT WAS IRRITABLE AND COMPLETELY CAME INTO CONSCIOUS,PT WAS PASSING 2-3 STOOLS /DAY
GCS-E4V3M6
DAY 9-
PT RESPONDED TO COMMANDS,ORIENTED TO TIME,PLACE,PERSON ,VITALS STABLE
SERUM AMMONIA 108(NORMAL)
RTPCR COVID NEGATIVE
3% NACL WAS STOPPED AND REST ALL OTHER TREATMENT WAS CONTINUED
AT AROUND 6 PM ,PT HAD 1 EPISODE OF ? ABSENCE SEIZURE WITH VISUAL HALLUCINATION
DAY 10-
ACUTE FULMINANT HEPATIC FAILURE SCONDARY TO ? POST INFECTIOUS(BACTERIAL/VIRAL)? TOXIN MEDIATED ? MISC WITH HEAPTIC ENCEPHALOPATHY RESOLVED
COAGULOPATHY REOLVED ,DKA RESOLVED ,THROMBOCYTOPENIA RESOLVING WITH METABOLIC SEIZURES
PT SLEPT WELL YESTERDAY NIGHT .NO EPISODES OF ABSENCE SEIZURES,NO HALLUCINATIONS ,PASSED STOOLS 2 TIMES YESTERDAY AND ONCE TODAY MRNG
SERIAL LFT MONITORING WAS DONE(TB 12)
DAY 11-
PT HAD NO COMPLAINTS
N ACETYL CYTEINE WAS CONVERTED TO TAB FORM,PT WAS AMBULATED ,REST ALL OTHER TREATMENT CONTINUED
DAY 12-
NO FRESH COMPLAINTS ,PASSED STOOLS 2 TIMES PER DAY ,SAME TREATMENT CONTINUED
DAY 13,14,15-
NO FRESH COMPLAINTS, PASSED STOOLS 2-3 TIMES A DAY,SAME TREATMENT CONTINUED AND VITALS STABLE
DAY 16-
ON THE DAY OF DISCHARGE ,PT IS CONSCIOUS ,COHERENT AND VITALS STABLE
TB 4.08, DB 3.62,AST 51,ALT 142, ALP 205, TP 6.6, ALB 2.9
PT WAS ADVISED TO TAKE EGG WHITES ,TO PASS STOOLS 2-3 TIMES /DAY AND REVIEW AFTER 1 WEEK WITH CBP,LFT,PT INR AND APTT
ADVICE AT DISCHARGE-
ORAL FLUIDS 2-3 LTS/DAY
TAB LEVIPIL 500 MG BD
TAB.UDILIV 300 MG BD FOR 5 DAYS
TAB.RIFAGUT 550 MG BD
TAB PANTOP 40 MG OD
SYP. HEPAMERZ 10 ML BD
SYP LACTULOSE 10 ML BD( TO PASS 2-3 STOOLS /DAY)
INJ. HAI SC 6U TID